Laser Therapy via Photobiomodulation for Musculoskeletal Pain in Clinical Settings
Musculoskeletal pain affects approximately 1.71 billion people worldwide annually[1] and is one of the most common reasons an individual may visit a physician for help.
Currently, the most common strategies to relieve musculoskeletal (MSK) pain is the use of non-steroidal anti-inflammatory drugs, steroidal injections, and opioid analgesics, each of which carries its own benefits, risks and undesirable adverse effects.[2]
However, over the past decade, there have been many advancements in technology to help reduce MSK pain without the use of medications. One of these technologies adopted across the medical community is light therapy, which has been shown to be effective in treating chronic and acute musculoskeletal conditions. This is achieved through a process called Photobiomodulation (PBM) using a light emitted from a ‘laser’, the acronym being Light Amplification by Stimulated Emission of Radiation.
Lasers imparting light into tissue to promote PBM may seem like something out of a science fiction movie, but there is an ever-growing body of research into this area. As of 2020, there are over 7500 published papers on PubMed on Low-Level Laser Therapy (LLLT) and over 1200 published articles on photobiomodulation. While the quality and size of these studies may vary, it’s clear that using laser therapy to treat musculoskeletal pain is not a fad nor fiction.
The development of common terminology
Several terms have been used to describe the effects that light therapy has on humans including Cold Laser Therapy, Biostimulation and Low-Level Laser Therapy (LLLT). Only within the last few years has there been a recent consensus from researchers and clinicians to migrate to the common term ’photobiomodulation‘ to describe light and its therapeutic application. In 2015, the term ‘photobiomodulation’ was formally added to the National Library of Medicine MeSH database as an official term to the existing record of laser therapy.[3]
What is Photobiomodulation (PBM) and how do lasers achieve it?
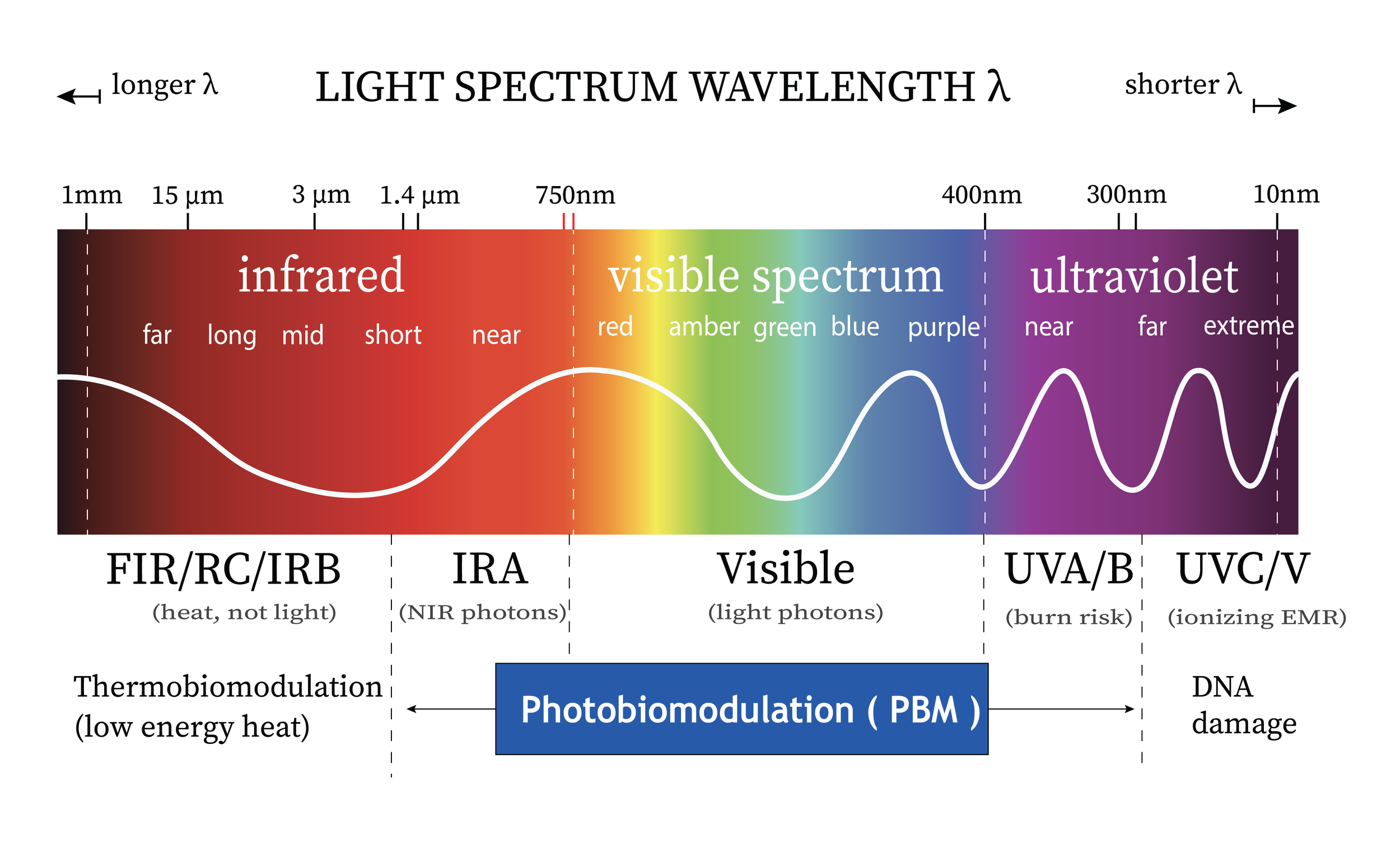
Photobiomodulation (PBM) is the biochemical reaction that occurs naturally in all living cells (including humans) in response to light within the infrared, near infrared, and visible light spectrum.
Light, such as sunlight contains energy particles called photons. When photons are transmitted and absorbed by living tissues, they provide energy to the cell’s mitochondria and organelles to stimulate cellular growth, metabolism, and in turn, accelerate healing processes and DNA repair. Two examples of light energy generating a photochemical reaction would be sunlight being absorbed by our skin to generate Vitamin D as well as the process of photosynthesis in plants. In plants, light is absorbed by the photoreceptor chlorophyl which helps convert CO2 to oxygen and drives on growth in the plant’s cellular structures.[4]
In humans, PBM has been shown in recent systematic reviews and meta-analyses to help improve wound and soft tissue healing, improve muscle regeneration, reduce inflammatory processes, and provide relief to both acute and chronic musculoskeletal pain syndromes.[5] Using light therapy via PBM can assist the body to repair itself, reduce pain by reducing inflammation, and aid healing.[6]
Although the process of PBM can occur superficially at the skin, for PBM to take place in tissues beneath the epidermis, specific wavelengths at higher power density (irradiance) need to be applied for calculated amounts of time to have an impact on different target tissues. High power therapeutic lasers have been designed to work in this capacity. How effectively light energy penetrates and is absorbed by the human body depends on several factors specific to both the laser and tissue being treated. One of the key laser components regarding the depth of penetration is wavelength, which is measured in nanometres or ’nm‘.
As a general rule, higher wavelengths in the near infrared spectrum can reach deeper tissues as they are less likely to be absorbed by the melanin in our skin.[7] Whilst the wavelength determines the depth of penetration, the power of the laser (measured in Watts) determines how much light energy is transmitted into the cells per second.
The therapeutic window for PBM occurs between the non-ionising wavelengths of 400nm up to the 1400nm. Non-ionising wavelengths are the wavelengths that do not carry enough energy to remove electrons from an atom or molecule. As they do not cause ionisation, they do not damage cells or DNA.[8] In contrast, wavelengths below the 400nm wavelength such as harmful ultraviolet (UV) light (UVA and UVB), can damage DNA and can pose a serious health hazard.
Unlike sunlight, which contains harmful UVA and UVB wavelengths, lasers can be programmed to emit safe and therapeutic non-ionising wavelengths between 400nm and 1400nm which helps stimulate growth, DNA repair and cellular metabolism.
How does light energy increase cellular metabolism in deep tissues?
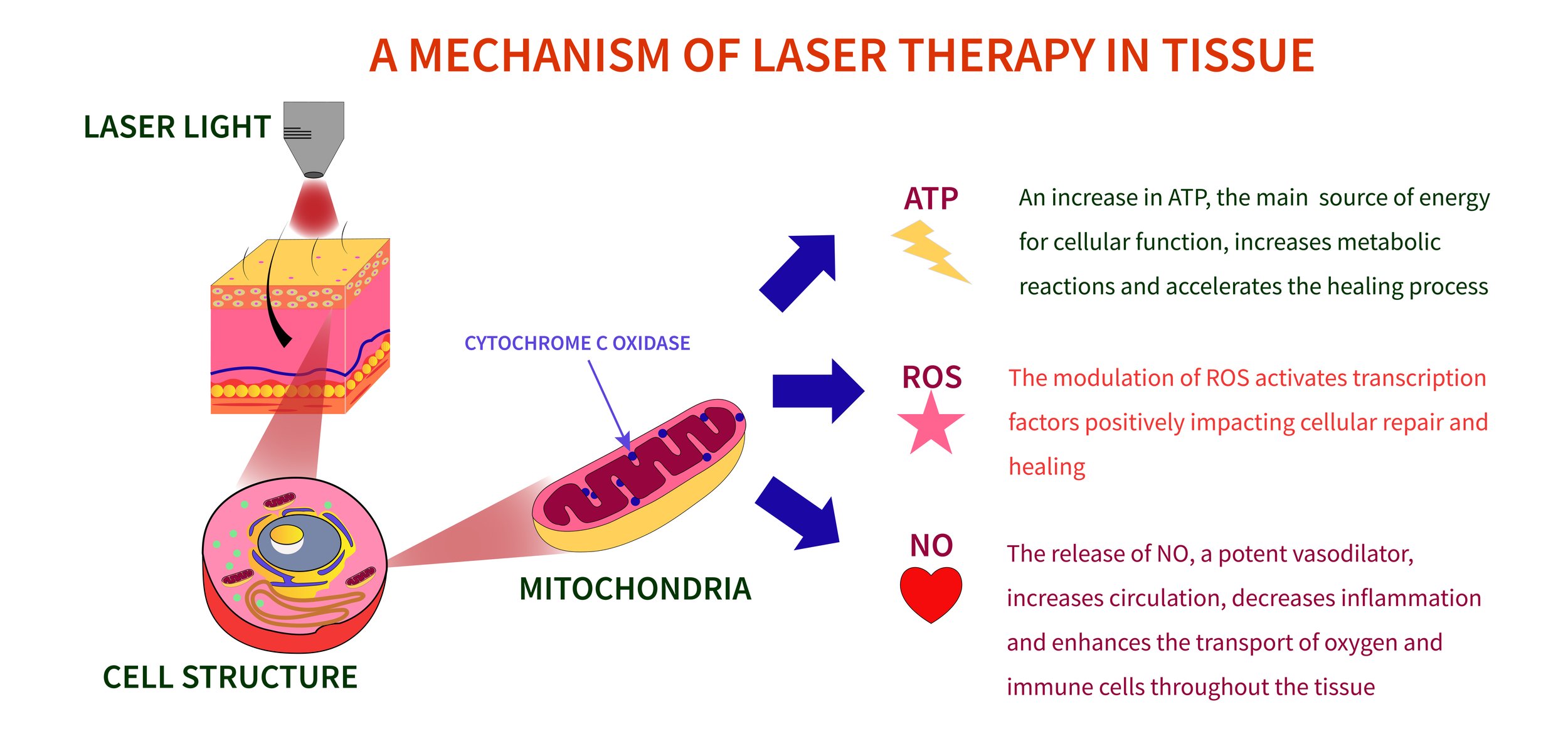
When light penetrates the body’s tissue at specific wavelengths, it reaches the mitochondria of the cell. Mitochondria are often referred to as the cell’s powerhouse, as they convert food into chemical energy to power the cell’s biochemical functions. The primary target for PBM is the cytochrome C complex which is found in the inner membrane of the mitochondria. Cytochrome C is a vital component of the mitochondria that drives cellular metabolism. The absorption of light stimulates Cytochrome C within the mitochondria, leading to increased production of adenosine triphosphate (ATP), which is the energy molecule that powers all the cells and metabolic activity in the body. Without ATP cells cannot survive. The increase in ATP production accelerates the function and repair processes of the cell.[9]
In addition to increased production of ATP, laser stimulation also produces free nitric oxide. Nitric oxide passes out of the cell and acts as a vasodilator, which means that it encourages blood flow into the surrounding areas. This extra blood flow into the damaged tissue delivers oxygen, vital sugars, proteins and salts and removes waste products, all of which accelerate cellular reproduction and growth, thereby aiding the healing process. These cellular processes translate into increased blood flow and reduced inflammation which may lead to reduced pain.
What is the ideal wavelength for therapeutic benefit?
As light energy travels through tissue, photons will either be reflected, scattered, absorbed or transmitted depending upon the characteristics of the tissue. For example, light can be absorbed by water, blood and the melanin of the skin. If sufficient light is unable to reach the targeted tissue, there will be no therapeutic change.[10] The optimal window or range of wavelengths through which light can penetrate tissue is referred to as the therapeutic window. Wavelengths of light in the near-infrared spectrum between 700 and 1300 nm are within the therapeutic window and are commonly used for PBM. However, research has shown that 810nm and 980nm are two of the most effective wavelengths when targeting PBM. [11] This is due to their ability to penetrate past the melanin layer of the skin and reach deeper tissues without being overly absorbed by water and blood in the body.
Light that is not overly absorbed by water or blood can penetrate much deeper than yellow, blue or other red wavelengths, producing results that assist with pain management due to the stimulation of nerve endings in the dermal layer of skin. [12]
Laser therapy light with 810nm and 980nm wavelengths also leads to upregulation of mitochondrial activity through increasing the mitochondrial response chain. This in turn increases ATP production into muscle cells and reduces oxidative stress. Research has shown that administering laser therapy of these wavelengths before exercise enhances performance and protects skeletal muscle against damage and inflammation.[13] Studies have also shown that these wavelengths lead to increased circulation and vasodilation, which assists with the healing process. Lasers using these wavelengths have been shown to be best suited for treating deep soft tissue injures such as muscle, deep fascia, and ligaments. [14][15][16]
Pulsed versus continuous laser therapy for PBM
There has been some debate as to which is more effective — pulsed or continuous laser therapy for PBM. It was previously reported that super pulsing 904nm wavelength light achieved greater penetration of biological tissues. However, research has shown that this is not the case. The effectiveness of laser therapy is dependent upon the dosage of energy delivered to the tissues rather than the mode of delivery. Super pulsing lasers deliver very little energy into tissues. A study comparing the energy penetration of a continuous emission 810nm laser with a 904nm super pulsed laser, at various time intervals showed the continuous emission laser allowed for greater energy to be delivered into the biological tissues in the measured time frame.[17] This is because super pulsing requires a longer warm-up time to deliver the same energy compared with continuous emission laser.
To achieve the same effects as a continuous emission laser, pulsed lasers require longer treatment times, in order to deliver the same dose of energy. Unfortunately, pulsed lasers use a diode that tends to overheat if left to fire continuously. Super pulsing prevents this overheating. As a consequence, super pulsing the laser means that the therapeutic effect of the laser is compromised as the tissue does not receive the correct dosage of energy until it is sufficiently warmed up. It’s for this reason that continuous laser therapy is the preferred mode of treatment for PBM.
Effectiveness of PBM for musculoskeletal conditions
Studies into the effectiveness of PBM have shown that it is an effective treatment for several musculoskeletal conditions including neck pain[18], temporomandibular joint disorders[19][20], shoulder pain[21][22][23], elbow and joint pain[24], fibromyalgia[25], low back pain[26][27], sciatica[28][29], arthritis[30], sports injuries[31][32], soft tissue damage[33], and plantar fasciitis.[34]
PBM has also been shown to be an effective, non-invasive, solution to help reduce inflammation without the side effects of medication. [35][36] In the US market, the Food and Drug Administration (FDA) has approved therapeutic laser for temporary relief of minor muscle and joint pain, muscle spasm, pain and stiffness associated with arthritis and promoting relaxation of the muscle tissue. In Australia the Therapeutic Goods Administration (TGA) has also approved it for the same applications.
There continues to be a growing body of peer-reviewed, clinical research, including numerous randomised control trials supporting the use of PBM in treating a large number of conditions. There are currently no known significant side effects reported with the use of laser therapy, making it an effective and well-tolerated primary or adjunct treatment for musculoskeletal injuries by the majority of patients.
Acknowledgement
I would like to acknowledge and thank Nerissa Bentley, of The Melbourne Health Writer for her contribution to this paper. Her outstanding research skills, thorough knowledge of the Australian Health Practitioner Regulation Agency (AHPRA) Advertising Guidelines, and her ability to translate complex medical information into easy-to-read copy have been pivotal in helping write this paper.
References:
[1]Cieza, A., Causey, K., Kamenov, K., Hanson, S. W., Chatterji, S., & Vos, T. (2020). Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10267), 2006-2017https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32340-0/fulltext
[2] Deeks ED. Fixed-dose ibuprofen/famotidine: a review of its use to reduce the risk of gastric and duodenal ulcers in patients requiring NSAID therapy.Clin Drug Investig.2013;33(9):689–697.https://pubmed.ncbi.nlm.nih.gov/23881568/
[3]American Society for Laser Medicine & Surgery, Photobiomodulation, https://www.aslms.org/for-the-public/treatments-using-lasers-and-energy-based-devices/photobiomodulation
[4] National Geographic Society, Photosynthesis, https://www.nationalgeographic.org/encyclopedia/photosynthesis/
[5] Gomes Teles, Ramon & Teles, Gomes & Dutra, Yago & Vale, Donária & Pereira, Thiago & Santos, Dos & Carlos, José & Neto, Raposo & Brito, Tarcisio & Costa, Mariana & Oliveira, Saul & Braúna, Isabela & Silva, Felipe & De, Marcelo & Filgueiras, Carvalho. (2018). Photobiomodulation in the Treatment of Muscle Injury: A Systematic Review. Critical Reviews in Physical and Rehabilitation Medicine. 30. 1-14. 10.1615/CritRevPhysRehabilMed.2018024861.
[6] Gomes Teles, Ramon & Teles, Gomes & Dutra, Yago & Vale, Donária & Pereira, Thiago & Santos, Dos & Carlos, José & Neto, Raposo & Brito, Tarcisio & Costa, Mariana & Oliveira, Saul & Braúna, Isabela & Silva, Felipe & De, Marcelo & Filgueiras, Carvalho. (2018). Photobiomodulation in the Treatment of Muscle Injury: A Systematic Review. Critical Reviews in Physical and Rehabilitation Medicine. 30. 1-14. 10.1615/CritRevPhysRehabilMed.2018024861.
[7] Ash C, Dubec M, Donne K, Bashford T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med Sci. 2017;32(8):1909-1918. doi:10.1007/s10103-017-2317-4, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5653719/
[8]Centers for Disease Control and Prevention, The Electromagnetic Spectrum: Non-Ionizing Radiation, https://www.cdc.gov/nceh/radiation/nonionizing_radiation.html
[9] Chris E. Stout, Matt Kruger and Jeffrey Rogers, (Eds)- © 2011 Bentham Science Publishers Ltd. Current Perspectives in Clinical Treatment & Management in Workers’ Compensation Cases, 2011, 15: 191-2.)
[10]Huang, Y. Biphasic Dose Response in Low Level Light Therapy. Dose Response. 2009; 7(4): 358–383.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790317/
[11] Wu X, Dmitriev AE, Cardoso MJ, Viers-Costello AG, Borke RC, Streeter J, Anders JJ. 810 nm Wavelength light: an effective therapy for transected or contused rat spinal cord. Lasers Surg Med. 2009 Jan;41(1):36-41. doi: 10.1002/lsm.20729. PMID: 19143019. https://pubmed.ncbi.nlm.nih.gov/19143019/
[12] Wu X, Dmitriev AE, Cardoso MJ, Viers-Costello AG, Borke RC, Streeter J, Anders JJ. 810 nm Wavelength light: an effective therapy for transected or contused rat spinal cord. Lasers Surg Med. 2009 Jan;41(1):36-41. doi: 10.1002/lsm.20729. PMID: 19143019. https://pubmed.ncbi.nlm.nih.gov/19143019/
[13]Aver Vanin A, De Marchi T, Tomazoni SS, Tairova O, LeãoCasalechi H, de Tarso Camillo de Carvalho P, Bjordal JM, Leal-Junior EC. Pre-Exercise Infrared Low-Level Laser Therapy (810 nm) in Skeletal Muscle Performance and Postexercise Recovery in Humans, What Is the Optimal Dose? A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Photomed Laser Surg. 2016 Oct;34(10):473-482. doi: 10.1089/pho.2015.3992. Epub 2016 Aug 29. PMID: 27575834.https://pubmed.ncbi.nlm.nih.gov/27575834/
[14]Enwemeka CS. Intricacies of dose in laser phototherapy for tissue repair and pain relief. Photomed Laser Surg. 2009 Jun;27(3):387-93. doi: 10.1089/pho.2009.2503. PMID: 19473073. https://pubmed.ncbi.nlm.nih.gov/19473073/
[15]Reddy GK. Photobiological basis and clinical role of low-intensity lasers in biology and medicine. J Clin Laser Med Surg. 2004 Apr;22(2):141-50. doi: 10.1089/104454704774076208. PMID: 15165389. https://pubmed.ncbi.nlm.nih.gov/15165389/
[16]Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Sanford LE, Woodruff LD. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004 Aug;22(4):323-9. doi: 10.1089/pho.2004.22.323. PMID: 15345176. https://pubmed.ncbi.nlm.nih.gov/15345176/
[17] Anders JJ, Wu X. Comparison of Light Penetration of Continuous Wave 810 nm and Superpulsed 904 nm Wavelength Light in Anesthetized Rats. Photomed Laser Surg. 2016 Sep;34(9):418-24. doi: 10.1089/pho.2016.4137. Epub 2016 Aug 8. PMID: 27500419., https://pubmed.ncbi.nlm.nih.gov/27500419/
[18]Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009 Dec 5;374(9705):1897-908. doi: 10.1016/S0140-6736(09)61522-1. Epub 2009 Nov 13. Erratum in: Lancet. 2010 Mar 13;375(9718):894. PMID: 19913903. https://pubmed.ncbi.nlm.nih.gov/19913903/
[19]Abbasgholizadeh ZS, Evren B, Ozkan Y. Evaluation of the efficacy of different treatment modalities for painful temporomandibular disorders. Int J Oral Maxillofac Surg. 2020 May;49(5):628-635. doi: 10.1016/j.ijom.2019.08.010. Epub 2019 Sep 21. PMID: 31547949. https://pubmed.ncbi.nlm.nih.gov/31547949/
[20]Khairnar S, Bhate K, S N SK, Kshirsagar K, Jagtap B, Kakodkar P. Comparative evaluation of low-level laser therapy and ultrasound heat therapy in reducing temporomandibular joint disorder pain. J Dent Anesth Pain Med. 2019 Oct;19(5):289-294. doi: 10.17245/jdapm.2019.19.5.289. Epub 2019 Oct 30. PMID: 31723669; PMCID: PMC6834715. https://pubmed.ncbi.nlm.nih.gov/31723669/
[21]Santamato A, Solfrizzi V, Panza F, Tondi G, Frisardi V, Leggin BG, Ranieri M, Fiore P. Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of people with subacromial impingement syndrome: a randomized clinical trial. Phys Ther. 2009 Jul;89(7):643-52. doi: 10.2522/ptj.20080139. Epub 2009 May 29. Erratum in: Phys Ther. 2009 Sep;89(9):999. PMID: 19482902. https://pubmed.ncbi.nlm.nih.gov/19482902/
[22]Kim SH, Kim YH, Lee HR, Choi YE. Short-term effects of high-intensity laser therapy on frozen shoulder: A prospective randomized control study. Man Ther. 2015 Dec;20(6):751-7. doi: 10.1016/j.math.2015.02.009. Epub 2015 Mar 2. PMID: 25770420. https://pubmed.ncbi.nlm.nih.gov/25770420/
[23]Awotidebe AW, Inglis-Jassiem G, Young T. Low-level laser therapy and exercise for patients with shoulder disorders in physiotherapy practice (a systematic review protocol). Syst Rev. 2015 Apr 30;4:60. doi: 10.1186/s13643-015-0050-2. PMID: 25925768; PMCID: PMC4423144. https://pubmed.ncbi.nlm.nih.gov/25925768/
[24] Roberts DB, Kruse RJ, Stoll SF. The effectiveness of therapeutic class IV (10 W) laser treatment for epicondylitis. Lasers Surg Med. 2013 Jul;45(5):311-7. doi: 10.1002/lsm.22140. Epub 2013 Jun 3. PMID: 23733499. https://pubmed.ncbi.nlm.nih.gov/23733499/
[25]Panton L, Simonavice E, Williams K, Mojock C, Kim JS, Kingsley JD, McMillan V, Mathis R. Effects of Class IV laser therapy on fibromyalgia impact and function in women with fibromyalgia. J Altern Complement Med. 2013 May;19(5):445-52. doi: 10.1089/acm.2011.0398. Epub 2012 Nov 23. PMID: 23176373. https://pubmed.ncbi.nlm.nih.gov/23176373/
[26]Alayat MS, Atya AM, Ali MM, Shosha TM. Long-term effect of high-intensity laser therapy in the treatment of patients with chronic low back pain: a randomized blinded placebo-controlled trial. Lasers Med Sci. 2014 May;29(3):1065-73. doi: 10.1007/s10103-013-1472-5. Epub 2013 Nov 2. https://pubmed.ncbi.nlm.nih.gov/24178907/
[27]Yousefi-Nooraie R, Schonstein E, Heidari K, Rashidian A, Pennick V, Akbari-Kamrani M, Irani S, Shakiba B, Mortaz Hejri SA, Mortaz Hejri SO, Jonaidi A. Low level laser therapy for nonspecific low-back pain. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD005107. doi: 10.1002/14651858.CD005107.pub4. PMID: 18425909.https://pubmed.ncbi.nlm.nih.gov/18425909/
[28]Holanda VM, Chavantes MC, Silva DF, de Holanda CV, de Oliveira JO Jr, Wu X, Anders JJ. Photobiomodulation of the dorsal root ganglion for the treatment of low back pain: A pilot study. Lasers Surg Med. 2016 Sep;48(7):653-9. doi: 10.1002/lsm.22522. Epub 2016 May 2. PMID: 27135465. https://pubmed.ncbi.nlm.nih.gov/27135465/
[29]Jovicić M, Konstantinović L, Lazović M, Jovicić V. Clinical and functional evaluation of patients with acute low back pain and radiculopathy treated with different energy doses of low level laser therapy. Vojnosanit Pregl. 2012 Aug;69(8):656-62. PMID: 22924260. https://pubmed.ncbi.nlm.nih.gov/22924260/
[30]Dima R, Tieppo Francio V, Towery C, Davani S. Review of Literature on Low-level Laser Therapy Benefits for Nonpharmacological Pain Control in Chronic Pain and Osteoarthritis. Altern Ther Health Med. 2018 Sep;24(5):8-10. PMID: 28987080. https://pubmed.ncbi.nlm.nih.gov/28987080/
[31]Alves AN, Fernandes KP, Deana AM, Bussadori SK, Mesquita-Ferrari RA. Effects of low-level laser therapy on skeletal muscle repair: a systematic review. Am J Phys Med Rehabil. 2014 Dec;93(12):1073-85. doi: 10.1097/PHM.0000000000000158. PMID: 25122099. https://pubmed.ncbi.nlm.nih.gov/25122099/
[32] Dornelles MP, Fritsch CG, Sonda FC, Johnson DS, Leal-Junior ECP, Vaz MA, Baroni BM. Photobiomodulation therapy as a tool to prevent hamstring strain injuries by reducing soccer-induced fatigue on hamstring muscles. Lasers Med Sci. 2019 Aug;34(6):1177-1184. doi: 10.1007/s10103-018-02709-w. Epub 2019 Jan 3. PMID: 30607719. https://pubmed.ncbi.nlm.nih.gov/30607719/
[33]Alves AN, Fernandes KP, Deana AM, Bussadori SK, Mesquita-Ferrari RA. Effects of low-level laser therapy on skeletal muscle repair: a systematic review. Am J Phys Med Rehabil. 2014 Dec;93(12):1073-85. doi: 10.1097/PHM.0000000000000158. PMID: 25122099.https://pubmed.ncbi.nlm.nih.gov/25122099/
[34] Ordahan B, Karahan AY, Kaydok E. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: a randomized clinical trial. Lasers Med Sci. 2018 Aug;33(6):1363-1369. doi: 10.1007/s10103-018-2497-6. Epub 2018 Apr 7. PMID: 29627888. https://pubmed.ncbi.nlm.nih.gov/29627888/
[35]Holanda VM, Chavantes MC, Silva DF, de Holanda CV, de Oliveira JO Jr, Wu X, Anders JJ. Photobiomodulation of the dorsal root ganglion for the treatment of low back pain: A pilot study. Lasers Surg Med. 2016 Sep;48(7):653-9. doi: 10.1002/lsm.22522. Epub 2016 May 2. PMID: 27135465. https://pubmed.ncbi.nlm.nih.gov/27135465/
[36]Holanda VM, Chavantes MC, Wu X, Anders JJ. The mechanistic basis for photobiomodulation therapy of neuropathic pain by near infrared laser light. Lasers Surg Med. 2017 Jul;49(5):516-524. doi: 10.1002/lsm.22628. Epub 2017 Jan 11. PMID: 28075022. https://pubmed.ncbi.nlm.nih.gov/28075022/