Disc Injuries (Disc Prolapse vs Disc Bulge)
What is Disc Injury?
Intervertebral discs are protective shock-absorbing pads between the bones of the spine (vertebrae). Disc injuries can occur from a variety of factors such as sports, lifting and rotating under a heavy load, or simply age-related degeneration.
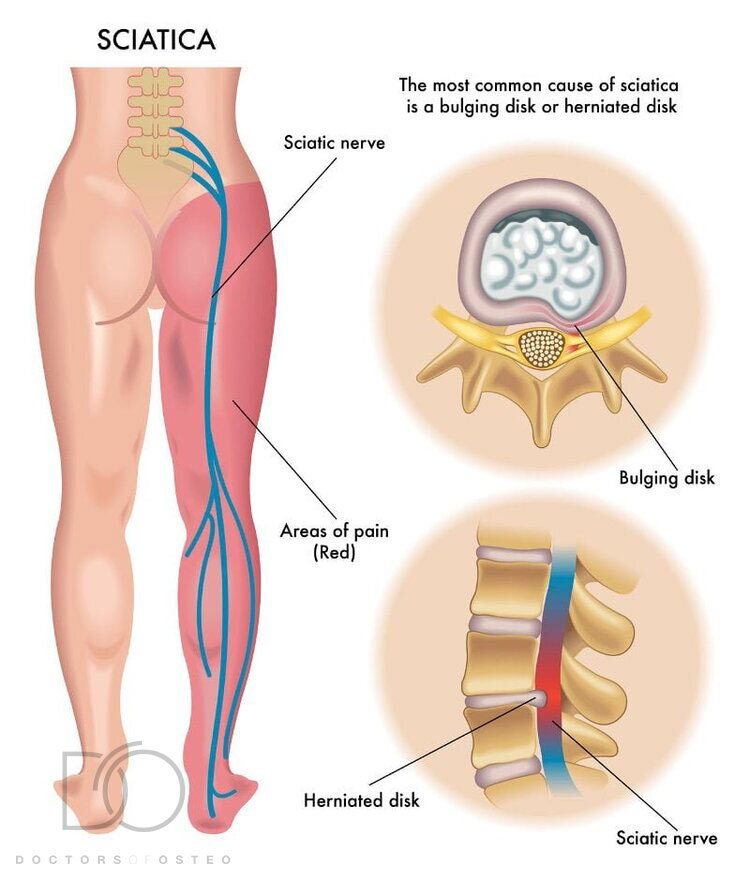
A disc may move, tear, or rupture, causing the outer annular cartilage and nearby tissue to fail, which in turn allows the inner gel portion of the disc to escape into the surrounding tissue. This leaking jelly-like substance can place pressure on the spinal cord or on an adjacent nerve to cause symptoms of sciatica such as pain down the leg, numbness, or weakness either around the damaged disc, or anywhere along the area supplied by that nerve.
What is the difference between a disc bulge, a disc prolapse and a disc herniation?
Broad-based disc bulge occurs when the inner gel portion of the disc extends outside the space it should normally occupy. The inner contents of the disc (nucleus pulposus) places pressure against a weak spot on the tough outer layer of cartilage (annulus fibrosus), resulting in a ‘bulged disc’. Although the bulging disc usually occupies 25-50% of the disc circumference, the disc is still contained within the annulus fibrosus.
Disc protrusions are similar to a bulged disc. However, the nucleus pulposus involves less than 25% of the disc circumference.
Herniated disc, also known as prolapsed disc or ‘slipped’ disc, is more severe, resulting in a tear or crack in the tough outer layer of cartilage which allows the softer inner cartilage to protrude out of the disc placing pressure on the nerves. Herniated discs are also called ruptured disks or slipped disks.
Bulging discs are more common and usually cause no pain. Herniated discs are more likely to cause pain, but some cause no pain whatsoever.
A disc sequestration is a progression of a herniated disc. The inner material of an intervertebral disc leaks through the tear in the outer layer and separates from the disc itself. The separated material may press onto nearby spinal nerves causing the common symptoms of pain, tingling, numbness or weakness.
How the body heals from disc injuries without treatment?
The cause of disc herniation, bulges or sequestrations is usually a tear in the annulus fibrosus that causes the nucleus pulposus to seep out. When this occurs, your body recognises the extruded nucleus pulposus as a material that should not come into contact with any other bodily tissues. Macrophages, a type of white blood cell, are released to break down the disc material until it can be completely resorbed by the body.
Most annular tears will close and heal within several weeks. Estimated time of recovery depends on the size of the herniation, whether or not it is impinging on any spinal nerves, as well as the patient’s own physiological factors (i.e. age, fitness levels, recurrence of disc injury).
What should you avoid doing?
Excessive activities should be avoided. While it is important to continue with normal activities as much as possible during your recovery, vigorous exercises should be kept to a minimum. It is paramount to discontinue any activities that aggravate your symptoms such as bending over, heavy lifting and any quick twisting or jerking motions. You should also avoid sitting for long periods of time as it may increase the strain on your spine.
At home, be cautious about low furniture and seats, as it may be difficult to stand back up after sitting. Do not lie on your stomach while you are sleeping – this position causes your spine to compress and irritate the disc injury further.
When surgery may be recommended?
If your symptoms do not reduce within 12 weeks of physical therapy, surgery may be recommended.
If you have a lot of wear and tear in the cartilage and collapse of the disc space, accompanied by pain that has no relief or improved function, then spinal surgery may be suggested only as a last resort to prevent further deterioration and pain.
At Doctors of Osteo, we can provide treatments to help manage symptoms associated with disc injuries.
How can Osteopathy help with a Disc Prolapse or Disc Bulge?
Osteopathy and other manual therapies may be beneficial in minor disc injuries, such as disc bulges. Osteopathic therapy can help relieve stiff and aching back muscles, which is a common secondary effect to disc injuries. Soft tissue therapy along with gentle osteopathic treatment may also alleviate symptoms of numbness and tingling down a spinal nerve.
Osteopathy may also be used to enhance the elimination of waste materials caused by the breakdown of the annular disc, during the reabsorption phase. Increasing blood flow and nutrients towards the site of injury is also vital to improve the healing process of a disc injury.
Your osteopath may also introduce certain stretching and strengthening exercises to improve your core muscles, which aim to reduce the strain that may be placed on your spine. Excess pressure on your disc injury may exacerbate the pain.
Doctors of Osteo provide quality disc prolapse treatments with our osteopaths near me in Hawthorn, Hawthorn East, Kew, Balwyn, Canterbury, Camberwell, Camberwell East, Richmond, Malvern and Glen Iris.